Read through (or scroll down) to the very end for more about Marcy.
I.
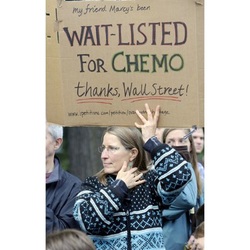
As the crowd of thousands marched downtown to the site of the Occupy Portland encampment, I left to run an errand. I’d been holding a handmade cardboard sign: “My friend Marcy is WAITLISTED FOR CHEMO – Thanks, Wall Street!” Many of the people reacting to my sign – whether supportive or averse – thought I was the one waiting for chemo. Even the AP photographer who snapped the picture of my sign that ended up on Internet sites around the world asked, “Is that about you?”
They thought I was the one with cancer. In the coming days, I began to wonder.
An hour after I left the rally, my belly began to feel like an air pump was inflating a basketball inside me. And I grew cold, so cold, despite my wool socks and heavy Guatemalan wool sweater. My teeth clacked and chattered. By the time I got home from my errands I had to unbutton the jeans that had required a tighter belt notch only that morning.
I forced my stiff, aching muscles up the stairs to my house and cocooned myself in a wool blanket in front of our fireplace. When the wracking chills still wouldn’t subside, my partner Amber found the thermometer. We were stunned when it registered 102.7 degrees. Must be broken. She took her own temperature – normal.
It was about 7:00 p.m. when I reached my doctor, who found it very odd: high fever and severe bloating, but no nausea, vomiting, or diarrhea, which you’d expect with food poisoning or a flu. We agreed that I’d try Tylenol and Gatorade and go to the ER if it got worse.
I woke up in the morning without a fever. But the bloating – I was still so unbearably full I found the idea of eating preposterous. I headed in to see my doctor. They took an abdominal X-ray and sent me home. Once they viewed the film, they wanted an ultrasound. I drove out in Friday afternoon rush hour having drunk the requisite 32 ounces of water – four tall glasses of liquid on top of the basketball in my belly. I was in agony.
I figured I ouldn’t get the results until Monday, but my doctor called and left a message around 6:00 p.m. It wasn’t a reassuring “all clear.” His voice sounded concerned. He told me to call him on Monday.
II.
Marcy’s unexpected diagnosis of Stage IV ovarian cancer had ripped the security blanket off our cozy community. In her early 50s, the poster child for effortless exercise and wholesome diet, Marcy exemplified clean country living. I had barely paused to admit my own emotional response to the pronouncement of her terminal disease. I had swung into action, attempting to impose order on this chaos by taking notes at her doctor’s appointments, organizing brigades of helpers, setting up communications systems.
The Monday morning after my ultrasound, I drove to Marcy’s house to accompany her and her husband, Mike, to see her surgeon, a highly respected gynecological oncologist on whom she had pinned her hopes.
During Marcy’s diagnosis 18 months earlier, Dr. C had gone in through her belly button to remove the small amounts of disease in her abdomen – debulking, they call it – but the cancer had already spread to her chest. Although the surgery and subsequent chemo had produced a blessed remission, her cancer holiday was over. The disease was clearly on the move once again. Marcy’s meeting with her medical oncologist had left her in despair. She wanted the surgeon to offer something more aggressive, to deliver some hope through scalpel and sutures.
Marcy wore one of her trademark loose skirts. Despite her willowy dancer’s frame she had always favored prairie skirts that allowed her unrestricted movement (and she was constantly in motion). Just before her diagnosis, she had shocked all of her friends by favoring chic new slim corduroy jeans. But the bloating that accompanied her chemo had become, in cancer-speak, her “new normal,” and now it was back to skirts. I was wearing a loose skirt that day, too, to ease the bloat in my own belly. And to hide it.
Over the weekend I’d received an email from one of the national ovarian cancer listservs I had subscribed to, promoting the checklist of early detection symptoms we all need to internalize, like the monthly breast self-exam we were trained to do in the early days of the pink-ribbon movement:
Symptoms of Ovarian Cancer
- Bloating
- Pelvic or abdominal pain
- Difficulty eating or feeling full quickly
- Urinary symptoms (urgency or frequency)
I was happy to stuff my own unknowns into the glove compartment for the morning; I preferred the immediacy of their fears to my own. I clamped down the impulse to distract us all with small talk or spiritual-silver-lining reassurances. We drove to the appointment in shared tense silence.
Marcy’s meeting with the surgeon delivered further devastation: he had nothing in his bag of tricks to help her. She fled the claustrophobic confines of the consultation room as soon as he left. I waited to get the paperwork and found Marcy and Mike in the parking lot. If I’d been unsure about conversation on the way there, I knew without a doubt there was nothing I could say now. Marcy was in full internal lockdown, desperate to be out of the car and back in her home doing the touchstone rituals she had devised to help her tolerate the intolerable.
As I pulled into the driveway she opened the door, “Sorry… rude…by myself.” She fled, with Mike not far behind her. I sat in my car getting her records release documents in order and offered a few inadequate words to Mike when he reemerged to fetch the documents. Then I pulled around the corner and called my doctor, expecting to hear reassurance in my ultrasound reading. Instead he told me there was a mass over my left ovary. He wanted an MRI to provide more detail. But first I should get to my gynecologist for an exam.
III.
Cancer World. It’s how writer Steven Shapin describes our modern existence in his review of the book “The Emperor of All Maladies: A Biography of Cancer” by physician Siddartha Mukherjee. Mukherjee calls cancer “the quintessential product of modernity.” Modern advancements mean more of us have cancer. We now outlive the diseases that killed our forebears before they had the chance to get the Big C. And the toxicity of our environment surely breeds more malignancy. How could it be coincidence that my father and his sister’s husband both died young of the same rare brain cancer, having shared no genetic link, only mutual employment in the family’s fuel tank cleaning business during my dad’s summer breaks from college and medical school?
Shapin, in The New Yorker (Nov. 8, 2010), argues that the modern impact of cancer goes beyond those who have the disease. He writes that historically, “The agonizing manner of cancer death was dreaded, but that fear was not centrally situated in the public mind—as it now is.” Shapin describes “two new kinds of beings in the modern cancer world.” One is the lucky patient who is now able to manage her once-fatal cancer as a chronic illness with miracle drugs like Gleevac. But Cancer World is also inhabited by the rest of us who are waiting and watching, “legions of the screened and the tested, who become more and more aware of the dangers battering away at their cells from the external environment and lurking inside, encoded in their genes.”
Just a month before my high fever and basketball belly, a surgeon excised a bad mole from my right tricep. The cells weren’t cancerous, but apparently that’s where they were headed. The mole is gone now, clean to the margins, but even in its absence, it increases my chances of developing a melanoma. So does the fact that my dad had a melanoma (separate from his brain cancer). And that my mom had another form of skin cancer, now known to be predictive of increased risk of the deadliest kind. My annual preventive visits to the dermatologist are now on a six-month schedule.
I’m a bit of an early detection nut. I’m not a hypochondriac (am I?); I don’t spend my time imagining myself filled with disease. But I don’t hesitate to call the doctor when I’m not sure what’s going on in my body. And I do every test they suggest.
I’m the daughter of a doctor, a man who knew he wanted to be a doctor as a young boy despite neither parent having graduated from high school. “He never went through the I-wanna-be-a-fireman-or-cowboy phase like the other little boys,” his older sister told me. “He just wanted to be a doctor.”
Thus I was born into my faith in the medical system. Not a blind faith: I believe that if you tell the doctor what’s going on, he or she will work with you to figure it out and will try to make you well or keep you safe. I have a strong sense of entitlement, being raised the daughter of a doctor, white and well-educated. They work for me, these doctors and diagnosticians. If I have questions, they will answer them.
And so I’ve been thoroughly probed and scanned and dissected. A lump removed from each breast in a procedure that strapped me to a narrow table, my arms pinned out to either side, crucifixion-style. A colonoscopy in my mid-40s. Suspicious moles carved out and shipped to the lab. X-rays, a CT scan, an MRI, and a PET scan to follow a nodule in my lung (nodule: another word for tumor, but writing tumor sounds melodramatic given its eventual disappearance).
And four years earlier I had been diagnosed with a bumper crop of uterine fibroids – inside my uterus; hanging from the outer wall on a stalk like a banana; embedded in the wall of my womb. Because I never had the heavy bleeding or cramping that plagues many women with such growths, the obvious solution, hysterectomy, seemed like overkill to me (fibroids are the leading cause of hysterectomy in the United States). But the bulk of my fibroids, equal to a six-month pregnancy, became tiresome. I felt obstructed from within when I did certain yoga poses, when I bent forward on my bicycle. My gynecologist warned of bowel and bladder difficulties; my chiropractor thought my breathing could be impaired and my skeletal system skewed.
I researched my options and opted for an embolization procedure to reduce the bulk without surgery. A radiologist inserted a catheter through my femoral artery and propelled microscopic pellets through it to block the blood flow from reaching the fibroids. I pictured them withering on the vine. A year later, my gynecologist reported with some amazement – she’d been a skeptic – that they had reduced in size by 50 percent, the optimal result expected from the procedure. Since then, I’d thought little about them, except during my annual pelvic exam as my gynecologist continued to marvel about the fibroids’ reduced dimensions.
IV.
The day after I accompanied Marcy on her futile pilgrimage to her cancer surgeon, I lay on my gynecologist’s exam table. She asked the question that seemed to solve the mystery of what had happened five days earlier.
“Did it feel like what you experienced when you had your embolization?” Yes, I realized, it was exactly like that. I don‘t know why it hadn’t occurred to me sooner. The procedure had involved an overnight stay in the hospital to control the high fever and severe pain that accompanies the death of the fibroid tissue when its blood supply is blocked. Now my gynecologist studied the original MRI that had guided the embolization and felt confident that it was consistent with the ultrasound that had alarmed the radiologist and my primary care physician. She would send both scans back to the radiologist to be sure.
It made sense to me now: some of the remaining fibroid tissue had gone into a death spiral. As it died – became necrotic, to get technical – the sanitation department kicked in. Fire up the incinerator (hello, 102.7 fever) and bring in the scrubbing bubbles of inflammation.
Still, I was relieved to get the call from my gynecologist three weeks later confirming that the radiologist had finally issued the all-clear. For now, anyway. The mass that had rung the alarm bell appeared consistent with the early pictures of the fibroids. But as with my dermatologist, my monitoring interval is now at the half-yearly rather than annual mark.
V.
My friend Marcy has cancer. I don’t. Yet. I belong to that tribe born of modern medical diagnostics: the precancerous. The Worried Well.
Six months after my belly bloat episode, on the eve of Marcy’s 53rd birthday and the second anniversary of her admittance to Cancer World, I joined her and three of her closest friends for a concert by N.E.D. “N.E.D. is cancer talk,” Marcy explained in her email invitation. “It’s what we all want to hear after a CT scan – that that we are No Evidence of Disease.” By definition, Stage IV cancer is considered incurable, so the women in Marcy’s cancer network strive instead to “dance with N.E.D”.
Made up of six full-time women’s cancer doctors from around the country, N.E.D.’s slogan is, “Breast cancer has a ribbon – but gynecological cancer has a rock band!” The theater buzzed with snappy women dressed for a party. The band started playing – original hard rock ballads belted out by the lone female doc, a hyper-athletic cross between Natalie Merchant and Janis Joplin – songs of love and heartbreak for the ovarian and uterine cancer patients whose disease inspires a rock band but very little funding for research.
They brandished their guitars and drums and microphones and filled our ears with the beat of the human drama – the full catastrophe as Zorba the Greek called it. Marcy and her three younger pals hit the dance floor and threw themselves into it, giddy, gossiping, mugging for photos. I couldn’t quite go there. My mind was busy worrying, calculating how I could get Marcy a doctor like one of those up there on the stage, a rock star doctor who would feel as passionately about saving her as I did. And my heart was stuck on the story she and a support-group friend had told us before the concert started. A year before when N.E.D. had come through town, the youngest member of their ovarian cancer group had shown up and danced her ass off. She’d been on her feet the whole show, having the time of her life. And then she’d gone home and died – that same night.
Anything can happen at any time. Watching all my risk factors – submitting to the twice-yearly exams and all the scans and probes, keeping my body strong, and eating as healthfully as I can – provides absolutely no guarantee that I won’t get cancer or any other illness. Maybe a serious illness isn’t even in my cards. I could get struck by a car and killed as I ride my bike to Marcy’s house.
I reside in what Shapin calls “the risk-factor world [which] holds out hope for avoiding cancer while recruiting masses of us into the anxious state of the ‘precancerous.’” The insurance companies know that’s my address, too. Because I’ve done all the diagnostic tests recommended to me, my only option for individual coverage, pre-Obamacare, was through the state high-risk pool.
My friend Marcy is dying. I’m dying too. We all are. She knows what’s going to be on her death certificate. I don’t. The lumps in my breasts, the moles, the fibroids, the solitary pulmonary nodule – they’re all benign, every one of them. So far.
During the episode of mysterious high fever and miserable cramping and the escalation of doctors’ concerns, I wasn’t afraid that I was going to die. I’m too good of a rational risk-calculator for that.
My fears reside at a deeper level. Am I big enough, small enough, brave enough, smart enough to proceed with open heart and open eyes through a world that gives Marcy cancer and me just a small dose of necrotic tissue? What sense can I make of a world that gives and takes away so randomly, that offers such exquisite beauty and love and joy and deals out such indiscriminate suffering? Can I make peace with a world that offers certainty, ultimately, about only one thing: my death, and the death of everyone I love?
Questions, I know, no MD or MRI can resolve.

Livingly Dying: Notes and Essays on Daily Life with Terminal Cancer



 RSS Feed
RSS Feed